Introduction
Living with diabetes requires a proactive and informed approach to health and wellness. It’s not just about managing blood sugar levels; it’s about embracing a holistic lifestyle that empowers you to thrive. In today’s fast-paced world, where information overload is common, understanding the core principles of healthy living with diabetes is more crucial than ever. This knowledge allows individuals to make informed decisions about their diet, exercise, and overall well-being, paving the way for a healthier and more fulfilling life.
The journey of healthy living with diabetes is personal and multifaceted, encompassing various aspects from nutritional choices to stress management. It’s about recognizing that diabetes management is not a one-size-fits-all solution but rather a customized plan tailored to individual needs and circumstances. By adopting a comprehensive approach that integrates medical advice with lifestyle modifications, individuals with diabetes can effectively manage their condition, reduce the risk of complications, and enhance their quality of life significantly.
This article serves as your comprehensive guide to healthy living with diabetes, offering practical strategies and evidence-based information to navigate your health journey successfully. We will delve into the essential components of a diabetes-friendly lifestyle, from crafting a balanced diet and incorporating regular physical activity to mastering blood sugar monitoring and stress reduction techniques. Our aim is to equip you with the knowledge and tools necessary to take control of your health and live a vibrant, healthy life with diabetes.
1. Understanding Diabetes and the Importance of Healthy Living
What is Diabetes?
Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disorder characterized by elevated blood sugar levels (hyperglycemia). This occurs when the body either doesn’t produce enough insulin (Type 1 diabetes) or can’t effectively use the insulin it produces (Type 2 diabetes). Insulin is a hormone produced by the pancreas that acts like a key, allowing sugar (glucose) from the food we eat to enter cells to be used for energy.
When insulin is lacking or ineffective, glucose builds up in the bloodstream, leading to a range of health problems over time. Gestational diabetes is another form that develops during pregnancy in some women, often resolving after childbirth but increasing the risk of type 2 diabetes later in life. Understanding the underlying mechanisms of diabetes is the first step towards embracing healthy living with diabetes.
Why is Healthy Living Crucial for Diabetes Management?
Adopting a healthy living with diabetes approach is not merely a suggestion but a cornerstone of effective diabetes management. It goes beyond just taking medication; it’s about actively participating in your health journey. Here’s why it’s so crucial:
- Blood Sugar Control: Healthy lifestyle choices, particularly diet and exercise, directly impact blood glucose levels. A balanced diet helps regulate the amount of glucose entering the bloodstream, while physical activity enhances insulin sensitivity and glucose uptake by cells. Effective blood sugar control minimizes the risks of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), both of which can be detrimental to health.
- Weight Management: Maintaining a healthy weight is often integral to managing Type 2 diabetes. Excess weight, especially around the abdomen, can worsen insulin resistance. Healthy living with diabetes strategies focus on sustainable weight management through balanced eating and regular exercise, which can significantly improve insulin sensitivity and overall metabolic health.
- Reduced Risk of Complications: Chronically high blood sugar can damage blood vessels and nerves over time, leading to serious long-term complications such as heart disease, stroke, kidney disease, nerve damage (neuropathy), eye damage (retinopathy), and foot problems. Healthy living with diabetes, including maintaining target blood sugar levels, blood pressure, and cholesterol, can significantly reduce the risk and progression of these complications.
- Improved Energy Levels and Well-being: Fluctuations in blood sugar can lead to fatigue and decreased energy levels. Healthy living with diabetes promotes stable blood sugar, leading to more consistent energy throughout the day and improved overall well-being. It also encompasses stress management and mental health, contributing to a more positive and balanced life.
- Enhanced Medication Effectiveness: Lifestyle modifications can often enhance the effectiveness of diabetes medications, potentially reducing the dosage required or even delaying or preventing the need for medication in some cases of prediabetes or early-stage Type 2 diabetes. Healthy living with diabetes works synergistically with medical treatments to achieve optimal health outcomes.
In essence, healthy living with diabetes is not just about managing a condition; it’s about empowering yourself to live a longer, healthier, and more fulfilling life. It’s about taking control and making informed choices that positively impact your well-being every day.
2. Nutrition: Fueling Your Body the Right Way for Diabetes
The Cornerstones of a Diabetes-Friendly Diet
Nutrition is arguably the most crucial pillar of healthy living with diabetes. A well-planned diet is not about deprivation or restrictive fad diets, but rather about making informed food choices that support blood sugar control, weight management, and overall health. The cornerstones of a diabetes-friendly diet emphasize whole, unprocessed foods that are nutrient-rich and naturally lower in added sugars and unhealthy fats. These cornerstones include:
- Non-Starchy Vegetables: These should form the foundation of your meals. Examples include leafy greens (spinach, kale, lettuce), broccoli, cauliflower, peppers, cucumbers, and tomatoes. They are low in calories and carbohydrates but packed with vitamins, minerals, and fiber.
- Lean Proteins: Choose lean sources of protein such as fish, poultry without skin, beans, lentils, tofu, and low-fat dairy. Protein helps with satiety, supports muscle mass, and has a minimal impact on blood sugar levels.
- Whole Grains: Opt for whole grains over refined grains. Examples include brown rice, quinoa, oats, whole wheat bread, and barley. Whole grains are rich in fiber, which helps slow down glucose absorption and promotes stable blood sugar.
- Healthy Fats: Incorporate sources of healthy fats such as avocados, nuts, seeds, olive oil, and fatty fish (salmon, tuna, mackerel). Healthy fats are essential for heart health and overall well-being.
- Fruits in Moderation: Fruits are naturally sweet but contain vitamins, minerals, and fiber. Choose fruits with lower glycemic index and consume them in moderation as part of a balanced meal. Examples include berries, apples, pears, and oranges.
Macronutrient Balance: Carbohydrates, Proteins, and Fats
Understanding macronutrient balance is key to crafting a diet that supports healthy living with diabetes.1 The three macronutrients—carbohydrates, proteins, and fats—each play distinct roles in the body, and their proportions in your diet significantly impact blood sugar2 levels and overall health.
- Carbohydrates: Carbohydrates are the primary source of energy for the body and have the most significant impact on blood glucose. However, not all carbohydrates are created equal. Focus on complex carbohydrates found in whole grains, vegetables, and fruits, which are digested more slowly and cause a gradual rise in blood sugar. Limit simple carbohydrates found in sugary drinks, processed foods, and refined grains, which are rapidly digested and can lead to blood sugar spikes.
- Proteins: Protein is essential for building and repairing tissues, and it has a minimal impact on blood sugar levels. Including protein in meals can help increase satiety and slow down the absorption of carbohydrates. Aim for lean protein sources in each meal.
- Fats: Healthy fats are crucial for heart health, brain function, and hormone production. Choose unsaturated fats (monounsaturated and polyunsaturated) found in olive oil, avocados, nuts, seeds, and fatty fish. Limit saturated and trans fats found in red meat, processed foods, and fried foods, as they can negatively impact cholesterol levels and heart health.
The ideal macronutrient ratio for healthy living with diabetes can vary based on individual needs and preferences, but a general guideline is to focus on a balanced intake with an emphasis on complex carbohydrates, lean proteins, and healthy fats, while carefully managing overall carbohydrate intake to maintain stable blood sugar levels. Consulting with a registered dietitian or certified diabetes educator can help personalize your macronutrient ratios.
Understanding the Glycemic Index and Load
The Glycemic Index (GI) and Glycemic Load (GL) are valuable tools for making informed food choices for healthy living with diabetes. They measure how quickly and how much a food raises blood glucose levels compared to pure glucose (or white bread).
- Glycemic Index (GI): The GI ranks carbohydrates on a scale of 0 to 100 based on how much they raise blood sugar levels after eating. High GI foods (70 or more) are digested and absorbed quickly, causing rapid blood sugar spikes. Medium GI foods (56-69) have a moderate effect, and low GI foods (55 or less) are digested and absorbed slowly, resulting in a gradual rise in blood sugar.
- Glycemic Load (GL): The GL takes into account both the GI of a food and the amount of carbohydrate per serving. It provides a more practical measure of a food’s impact on blood sugar in typical serving sizes. A GL of 10 or less is considered low, 11-19 is medium, and 20 or more is high.
While GI and GL are helpful guides, it’s important to consider other factors as well, such as portion size, cooking methods, and individual responses to food. Focusing on low to medium GI and GL foods as part of a balanced diet can contribute significantly to healthy living with diabetes by promoting stable blood sugar levels. Table 1 below provides examples of foods with varying GI and GL values.
Table 1: Examples of Foods with Glycemic Index (GI) and Glycemic Load (GL)
| Food | Serving Size | GI | GL |
| White Bread | 1 slice | 75 | 10 |
| Brown Rice | 1 cup cooked | 68 | 23 |
| Sweet Potato | 1 medium | 63 | 17 |
| Apple | 1 medium | 36 | 6 |
| Lentils | 1 cup cooked | 29 | 7 |
| Skim Milk | 1 cup | 32 | 4 |
Data sources: Harvard Health Publishing, American Diabetes Association.
Portion Control and Mindful Eating
Portion control and mindful eating are essential habits for healthy living with diabetes. Even healthy foods can raise blood sugar if consumed in excessive quantities.
- Portion Control: Being mindful of portion sizes helps manage overall calorie and carbohydrate intake. Use measuring cups and spoons initially to get accustomed to appropriate portion sizes. Choose smaller plates and bowls. Be aware of serving sizes listed on food labels.
- Mindful Eating: Mindful eating involves paying attention to your hunger and fullness cues, eating slowly and deliberately, and savoring each bite. It helps prevent overeating and promotes a healthier relationship with food. Practice eating without distractions (TV, phone). Listen to your body’s signals – eat when you’re truly hungry and stop when you’re satisfied, not stuffed.
Hydration: The Unsung Hero
Adequate hydration is often overlooked but plays a vital role in healthy living with diabetes. Water is essential for numerous bodily functions, including regulating blood sugar levels, transporting nutrients, and flushing out waste products.
- Benefits of Hydration: Drinking enough water helps dilute excess glucose in the bloodstream and supports kidney function, which is crucial for filtering out excess sugar. Dehydration can actually lead to higher blood sugar concentrations. Water also helps with energy levels and overall metabolic function.
- Recommended Fluid Intake: The general recommendation is to drink at least 8 glasses of water per day, but individual needs may vary based on activity level, climate, and overall health. Monitor your thirst and urine color (pale yellow is a good indicator of hydration).
- Diabetes-Friendly Beverages: Water is the best choice. Unsweetened tea, herbal tea, and black coffee are also good options. Avoid sugary drinks like soda, juice, and sweetened beverages, as they can drastically spike blood sugar levels.
Sample Meal Plan for Healthy Living with Diabetes
Table 2 provides a sample one-day meal plan for healthy living with diabetes. This is just an example, and individual meal plans should be tailored to personal preferences, dietary needs, and blood sugar goals. Consult with a registered dietitian or certified diabetes educator for personalized guidance.
Table 2: Sample Meal Plan for Healthy Living with Diabetes
| Meal | Example Foods |
| Breakfast | Oatmeal (1/2 cup cooked) with berries (1/2 cup) and nuts (1/4 cup), 1 hard-boiled egg |
| Lunch | Salad with grilled chicken or fish (4 oz), mixed greens, non-starchy vegetables, olive oil and vinegar dressing, whole-wheat roll (1 small) |
| Dinner | Baked salmon (4 oz) with roasted broccoli and quinoa (1/2 cup cooked) |
| Snacks | Apple slices with almond butter (2 tbsp), Greek yogurt (1 cup) with berries (1/4 cup), Handful of almonds (1 oz), Vegetable sticks (carrots, celery) with hummus (2 tbsp) |
This meal plan focuses on whole, unprocessed foods, lean proteins, healthy fats, and controlled portions of complex carbohydrates. It is designed to be balanced and nutritious, supporting healthy living with diabetes.
3. The Power of Physical Activity in Healthy Living with Diabetes
Benefits of Exercise for Diabetes Management
Regular physical activity is an indispensable component of healthy living with diabetes, offering a multitude of benefits that extend far beyond weight management. Exercise plays a crucial role in improving insulin sensitivity, controlling blood sugar, and reducing the risk of diabetes-related complications.
- Improved Insulin Sensitivity: Exercise makes your body more sensitive to insulin, meaning your cells become more receptive to glucose uptake. This allows insulin to work more effectively in lowering blood sugar levels. Even moderate physical activity can significantly improve insulin sensitivity.
- Blood Sugar Control: During exercise, muscles use glucose for energy, helping to lower blood sugar levels. Regular physical activity helps maintain stable blood sugar levels over time and can reduce A1c levels (a measure of average blood sugar over 2-3 months).
- Weight Management: Exercise burns calories, contributing to weight loss or maintenance. Achieving and maintaining a healthy weight is particularly important for managing Type 2 diabetes, as excess weight can worsen insulin resistance.
- Cardiovascular Health: People with diabetes are at higher risk of heart disease. Exercise strengthens the heart and improves cardiovascular health by lowering blood pressure, improving cholesterol levels, and reducing the risk of heart attack and stroke.
- Stress Reduction and Mood Enhancement: Physical activity is a natural stress reliever and mood booster. Exercise releases endorphins, which have mood-elevating effects. Managing stress is crucial for healthy living with diabetes, as stress can impact blood sugar levels.
Types of Exercise: Cardio, Strength Training, and Flexibility
A well-rounded exercise program for healthy living with diabetes should incorporate different types of activity to maximize benefits:
- Cardiovascular Exercise (Aerobic): Cardio activities raise your heart rate and breathing, improving cardiovascular health and burning calories. Examples include brisk walking, jogging, swimming, cycling, dancing, and hiking. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread throughout the week.
- Strength Training (Resistance Training): Strength training involves using resistance to build and maintain muscle mass. Muscle tissue is more insulin-sensitive than fat tissue, so increasing muscle mass can improve insulin sensitivity and glucose metabolism. Examples include lifting weights, using resistance bands, bodyweight exercises (push-ups, squats), and weight machines. Aim for strength training at least 2-3 times per week, working major muscle groups.
- Flexibility and Balance Exercises: Flexibility exercises, such as stretching and yoga, improve range of motion and prevent injuries. Balance exercises, such as tai chi or simply standing on one foot, can improve stability and reduce the risk of falls, which is particularly important for older adults with diabetes. Include flexibility and balance exercises in your routine several times a week.
Creating a Safe and Effective Exercise Plan
Creating a safe and effective exercise plan for healthy living with diabetes involves considering individual health status, fitness level, and any diabetes-related complications. It’s crucial to consult with your doctor before starting a new exercise program, especially if you have any pre-existing health conditions.
- Start Slowly and Gradually Increase Intensity: If you’re new to exercise, begin with short sessions of low-intensity activity and gradually increase the duration, intensity, and frequency as your fitness improves.
- Choose Activities You Enjoy: Select activities you find enjoyable and sustainable to increase adherence and long-term consistency. Variety can also help keep you motivated.
- Warm-up and Cool-down: Always include a warm-up before each workout to prepare your muscles and a cool-down afterwards to gradually lower your heart rate.
- Proper Footwear and Gear: Wear supportive shoes and appropriate clothing for your chosen activity to prevent injuries, especially foot problems, which are common in diabetes.
- Stay Hydrated: Drink plenty of water before, during, and after exercise to prevent dehydration.
Monitoring Blood Sugar Levels During Exercise
Monitoring blood sugar levels before, during, and after exercise is essential for healthy living with diabetes to understand how your body responds to different types of physical activity and to prevent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar) related to exercise.
- Check Blood Sugar Before Exercise: Check your blood sugar before starting any workout. If it’s below 100 mg/dL, you may need to have a small carbohydrate snack (e.g., fruit, crackers) before exercising to prevent hypoglycemia. If it’s above 250 mg/dL and you have ketones, it’s generally advised to postpone exercise until blood sugar is better controlled.
- Carry a Fast-Acting Carbohydrate: Always carry a source of fast-acting carbohydrate (glucose tablets, juice, hard candy) with you during exercise to treat hypoglycemia if it occurs.
- Monitor Blood Sugar During and After Exercise (especially initially): For longer workouts or new activities, you may want to check blood sugar during and after exercise to understand your body’s response and adjust your plan accordingly. Exercise can sometimes cause blood sugar to drop during or even several hours after the activity.
Staying Motivated and Consistent
Consistency is key to reaping the long-term benefits of exercise for healthy living with diabetes. Staying motivated can be challenging, but these strategies can help:
- Set Realistic Goals: Start with small, achievable goals and gradually increase them as you progress. Celebrate your milestones.
- Find an Exercise Buddy: Exercising with a friend or family member can provide mutual support and accountability.
- Join a Group Class or Fitness Program: Group exercise classes or diabetes-specific programs can provide structure, social support, and professional guidance.
- Track Your Progress: Keep a record of your workouts and blood sugar readings to monitor your progress and stay motivated.
- Reward Yourself (healthily): Celebrate your achievements with non-food rewards, such as new workout gear or a relaxing massage.
Incorporating regular physical activity into your routine is a powerful tool for healthy living with diabetes. It’s not just about exercise; it’s about moving towards a healthier, more energetic, and empowered you.
4. Blood Sugar Monitoring: Your Key to Proactive Diabetes Management
Why is Regular Blood Sugar Monitoring Essential?
Regular blood sugar monitoring is the cornerstone of proactive healthy living with diabetes. It provides real-time information about your blood glucose levels, empowering you and your healthcare team to make informed decisions about your diabetes management plan. It’s like having a window into how your body is responding to food, exercise, medication, stress, and illness.
- Personalized Diabetes Management: Diabetes affects everyone differently. Blood sugar monitoring allows for individualized adjustments to your diet, exercise, and medication regimen based on your unique blood sugar patterns.
- Understanding Food Effects: Monitoring before and after meals helps you see how different foods impact your blood sugar. This knowledge is invaluable for making informed dietary choices and optimizing your meal plans for healthy living with diabetes.
- Assessing Exercise Impact: Blood sugar monitoring around exercise allows you to understand how physical activity affects your glucose levels. This helps you plan your workouts safely and effectively, preventing hypoglycemia or hyperglycemia.
- Medication Adjustment and Optimization: Monitoring data helps your healthcare provider fine-tune your medication dosage or insulin regimen to achieve optimal blood sugar control. It allows for timely adjustments to address trends and patterns.
- Detecting and Preventing Hypoglycemia and Hyperglycemia: Regular monitoring enables early detection of both low and high blood sugar levels. Prompt action can be taken to correct these imbalances, preventing potentially dangerous symptoms and long-term complications.
- Tracking Progress and Motivation: Seeing your blood sugar readings improve over time can be incredibly motivating and reinforce positive lifestyle changes for healthy living with diabetes. It provides tangible evidence of your efforts and progress.
Types of Blood Sugar Monitoring Devices
Several types of blood sugar monitoring devices are available, ranging from traditional finger-prick methods to advanced continuous glucose monitoring systems.
- Blood Glucose Meters (BGMs): Traditional BGMs require a small blood sample obtained by pricking your fingertip with a lancet. The blood is then placed on a test strip inserted into the meter, which displays your blood sugar reading. BGMs are portable, relatively inexpensive, and widely accessible.
- Lancets and Lancing Devices: Lancets are small, sterile needles used to prick the skin. Lancing devices make the process easier and less painful.
- Test Strips: Test strips are specific to each type of meter and contain chemicals that react with glucose in the blood sample to produce a reading. They are a recurring cost associated with BGM use.
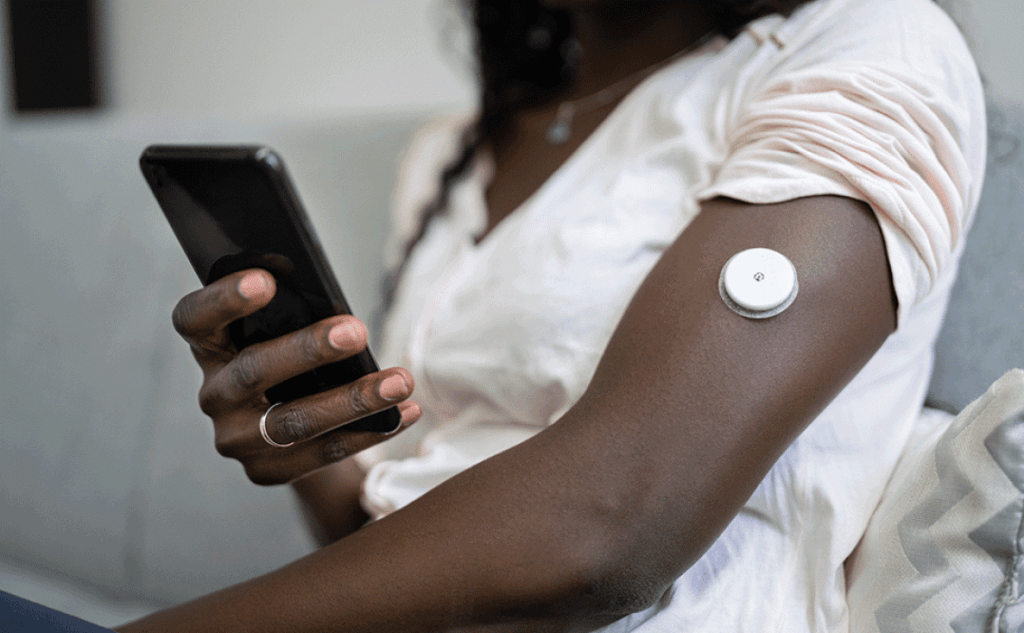
- Continuous Glucose Monitoring (CGM) Systems: CGMs are advanced devices that continuously track glucose levels in interstitial fluid (fluid under the skin) throughout the day and night. A small sensor is inserted under the skin, typically on the abdomen or arm, and transmits glucose data wirelessly to a receiver or smartphone. CGMs provide real-time glucose readings, trend arrows indicating glucose direction and rate of change, and alarms for high and low glucose levels. CGMs offer a more comprehensive picture of glucose patterns compared to BGMs. Figure 1 below illustrates a typical CGM system.
Figure 1: Continuous Glucose Monitoring (CGM) System
Understanding Your Blood Sugar Readings and Targets
Understanding your blood sugar readings and target ranges is crucial for effective healthy living with diabetes. Target ranges may vary slightly depending on individual factors and recommendations from your healthcare provider, but general guidelines are often used.
- Target Blood Sugar Ranges (General Guidelines):
- Before Meals (Fasting): 80-130 mg/dL (4.4-7.2 mmol/L)
- 1-2 Hours After the Start of a Meal (Postprandial): Less than 180 mg/dL (10.0 mmol/L)
- A1c (Hemoglobin A1c): Less than 7% (for many adults)
- Hypoglycemia (Low Blood Sugar): Hypoglycemia is typically defined as blood sugar below 70 mg/dL (3.9 mmol/L). Symptoms can include shakiness, sweating, dizziness, confusion, and hunger. It’s important to treat hypoglycemia promptly with fast-acting carbohydrates.
- Hyperglycemia (High Blood Sugar): Hyperglycemia refers to blood sugar levels above target ranges. Symptoms can include increased thirst, frequent urination, fatigue, and blurred vision. Persistent hyperglycemia needs to be addressed to prevent long-term complications.
- Time in Range (TIR): CGM systems often focus on “Time in Range,” which is the percentage of time glucose levels are within the target range (typically 70-180 mg/dL). Aiming for a higher TIR is associated with better long-term outcomes.
Tips for Effective Blood Sugar Monitoring
Effective blood sugar monitoring for healthy living with diabetes involves more than just checking your levels; it includes proper technique, data interpretation, and communication with your healthcare team.
- Follow Meter Instructions: Always use your blood glucose meter and test strips according to the manufacturer’s instructions to ensure accurate readings.
- Proper Blood Sampling Technique: Wash your hands before testing. Use a fresh lancet for each test. Prick the side of your fingertip for less pain. Obtain an adequate blood sample size for the test strip.
- Record Your Readings: Keep a logbook or use a digital app to record your blood sugar readings, along with meal times, exercise, medication, and any relevant notes (stress, illness). This data helps identify patterns and trends.
- Understand Factors Affecting Blood Sugar: Learn how various factors like food, exercise, stress, illness, and medications influence your blood sugar levels. This knowledge empowers you to make informed lifestyle adjustments.
- Regularly Review Data with Your Healthcare Team: Share your blood sugar logs or CGM data with your doctor, certified diabetes educator, or registered dietitian during appointments. They can help you interpret the data, adjust your management plan, and address any challenges.
Continuous Glucose Monitoring (CGM): A Technological Advancement
Continuous Glucose Monitoring (CGM) has revolutionized healthy living with diabetes by providing a dynamic and comprehensive view of glucose patterns. CGM offers several advantages over traditional BGM:
- Real-Time Glucose Readings: CGMs provide glucose readings every few minutes, giving you a continuous stream of data rather than just snapshots at specific times.
- Trend Arrows and Rate of Change: CGM systems display trend arrows indicating the direction and speed of glucose changes, allowing you to anticipate and proactively manage fluctuations.
- Alerts and Alarms: CGMs can be set to alert you when glucose levels are too high or too low, even at night, providing an added layer of safety.
- Data Analysis and Reporting: CGM data can be easily downloaded and analyzed to identify patterns, track progress, and generate reports for healthcare providers.
- Reduced Need for Fingersticks: CGM significantly reduces the need for routine fingerstick blood glucose checks. While occasional fingersticks may still be needed for calibration or confirmation, CGM greatly minimizes finger-prick burden.
CGM technology is continually advancing, becoming more accurate, user-friendly, and integrated with insulin pumps and smartphone apps. While CGM may not be necessary or suitable for everyone with diabetes, it is a powerful tool for many individuals seeking tighter glucose control and improved healthy living with diabetes.
5. Stress Management and Mental Well-being for Healthy Living with Diabetes
The Impact of Stress on Blood Sugar Levels
Stress is an unavoidable part of life, but chronic stress can have a significant negative impact on healthy living with diabetes. When you experience stress, your body releases stress hormones, such as cortisol and adrenaline. These hormones can cause the liver to release stored glucose into the bloodstream, leading to elevated blood sugar levels. Stress hormones can also make your body less sensitive to insulin, further contributing to hyperglycemia.
- Stress Hormones and Glucose Release: Cortisol and adrenaline signal the liver to produce and release glucose to provide energy for a “fight or flight” response. This physiological response, while helpful in acute situations, can become problematic when stress is chronic, leading to consistently elevated blood sugar.
- Insulin Resistance: Chronic stress can contribute to insulin resistance, making it harder for insulin to effectively lower blood sugar. This can worsen hyperglycemia in individuals with diabetes.
- Unhealthy Coping Mechanisms: Stress can sometimes lead to unhealthy coping behaviors, such as emotional eating, skipping exercise, or neglecting medication, all of which can negatively impact blood sugar control and healthy living with diabetes.
Stress Reduction Techniques: Mindfulness, Meditation, and Yoga
Incorporating stress reduction techniques into your daily routine is crucial for healthy living with diabetes. Mindfulness, meditation, and yoga are evidence-based practices that can effectively reduce stress, promote relaxation, and improve mental well-being.
- Mindfulness: Mindfulness involves paying attention to the present moment without judgment. Mindfulness techniques can include focused breathing exercises, body scan meditations, and mindful awareness of daily activities. Mindfulness helps reduce stress reactivity and promotes emotional regulation.
- Meditation: Meditation is a practice that involves training your mind to focus and quiet thoughts. Various meditation techniques exist, such as guided meditation, transcendental meditation, and loving-kindness meditation. Regular meditation can reduce stress hormones, lower blood pressure, and improve overall mood.
- Yoga: Yoga combines physical postures, breathing techniques, and meditation or relaxation. Yoga can reduce stress, improve flexibility and balance, and promote relaxation. Specific yoga poses and breathing exercises are particularly beneficial for stress reduction. Figure 2 shows an example of a yoga pose that can be helpful for stress reduction.
Figure 2: Yoga Pose for Stress Reduction (Child’s Pose)

Prioritizing Sleep and Rest
Adequate sleep and rest are often underestimated but are vital for healthy living with diabetes. Sleep deprivation and poor sleep quality can disrupt hormone balance, increase stress hormones, and impair insulin sensitivity, all of which can negatively affect blood sugar control.
- Sleep Duration and Quality: Aim for 7-8 hours of quality sleep per night. Establish a regular sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment (dark, quiet, cool room).
- Sleep Apnea Screening: Sleep apnea, a condition characterized by pauses in breathing during sleep, is more common in people with diabetes. Sleep apnea can worsen insulin resistance and increase cardiovascular risk. If you experience symptoms like loud snoring, daytime sleepiness, or gasping for air during sleep, discuss sleep apnea screening with your doctor.
- Rest and Relaxation: In addition to sleep, incorporate regular rest and relaxation periods into your day. Take short breaks during work or activities to relax and de-stress. Engage in enjoyable hobbies and activities that promote relaxation.
Building a Support System
Having a strong support system is invaluable for healthy living with diabetes. Diabetes management can be challenging, and having supportive relationships can make a significant difference in your emotional well-being and ability to cope with the demands of living with diabetes.
- Family and Friends: Educate your family and friends about diabetes and how they can support you. Open communication and understanding from loved ones can provide emotional comfort and practical assistance.
- Diabetes Support Groups: Joining a diabetes support group, either online or in person, provides an opportunity to connect with others who understand the challenges of living with diabetes. Sharing experiences, tips, and emotional support within a community can be empowering and reduce feelings of isolation.
- Healthcare Team Support: Build a strong relationship with your healthcare team, including your doctor, certified diabetes educator, registered dietitian, and mental health professional if needed. Regular communication and collaboration with your healthcare team are essential for optimal diabetes management and support.
Seeking Professional Mental Health Support
Diabetes can sometimes increase the risk of mental health challenges, such as anxiety and depression. Don’t hesitate to seek professional mental health support if you are struggling with emotional distress related to diabetes or general mental health concerns.
- Therapy and Counseling: Therapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy (IPT), can help you develop coping skills for stress, anxiety, and depression. Therapy can also provide a safe space to process emotions related to living with a chronic condition like diabetes.
- Medication for Mental Health Conditions: If you are diagnosed with anxiety or depression, medication may be a helpful component of your treatment plan. Discuss medication options with your doctor or a psychiatrist.
- Integrated Mental Health Care: Ideally, mental health care should be integrated into your overall diabetes care. Some diabetes clinics have mental health professionals as part of their multidisciplinary teams.
Prioritizing stress management and mental well-being is an integral aspect of healthy living with diabetes. By incorporating stress reduction techniques, prioritizing sleep, building a support system, and seeking professional mental health help when needed, you can enhance your emotional well-being and improve your overall diabetes management outcomes.
6. Medication and Insulin Therapy in Diabetes Management
Understanding Different Diabetes Medications
Medication plays a crucial role in managing diabetes for many individuals, particularly in Type 2 diabetes where lifestyle modifications alone may not be sufficient to achieve target blood sugar levels. Various classes of diabetes medications are available, each working in different ways to lower blood glucose. The choice of medication depends on the type of diabetes, individual health factors, and treatment goals.
- Metformin: Metformin is often the first-line medication for Type 2 diabetes. It works primarily by reducing glucose production in the liver and improving insulin sensitivity. Metformin is generally well-tolerated and has a low risk of hypoglycemia when used alone.
- Sulfonylureas: Sulfonylureas, such as glipizide and glimepiride, stimulate the pancreas to release more insulin. They can be effective in lowering blood sugar but carry a higher risk of hypoglycemia compared to metformin.
- DPP-4 Inhibitors: DPP-4 inhibitors, such as sitagliptin and linagliptin, help increase insulin release and decrease glucagon secretion in response to food intake. They have a lower risk of hypoglycemia than sulfonylureas and are generally well-tolerated.
- SGLT2 Inhibitors: SGLT2 inhibitors, such as canagliflozin and empagliflozin, work by increasing glucose excretion in the urine. They can lower blood sugar, promote weight loss, and have cardiovascular benefits.
- GLP-1 Receptor Agonists: GLP-1 receptor agonists, such as liraglutide and semaglutide, mimic the effects of a natural hormone called GLP-1, which stimulates insulin release, slows gastric emptying, and reduces appetite. They are effective in lowering blood sugar, promoting weight loss, and have cardiovascular benefits. Some are available in oral form, while others are injectable.
- Thiazolidinediones (TZDs): TZDs, such as pioglitazone, improve insulin sensitivity in muscle and fat tissue. They are effective in lowering blood sugar but have potential side effects, including weight gain and fluid retention.
Insulin Therapy: When and How it’s Used
Insulin therapy is essential for individuals with Type 1 diabetes, as their bodies do not produce insulin. Insulin is also often needed in Type 2 diabetes when other medications are not sufficient to achieve target blood sugar control. Insulin must be administered by injection or infusion as it cannot be taken orally.
- Types of Insulin: Various types of insulin are available, categorized by their onset, peak, and duration of action:
- Rapid-acting insulin: Starts working quickly (within minutes), peaks in about an hour, and lasts for 2-4 hours. Used to cover meals and correct high blood sugar.
- Short-acting insulin (Regular insulin): Starts working within 30 minutes, peaks in 2-3 hours, and lasts for 3-6 hours. Typically taken before meals.
- Intermediate-acting insulin (NPH insulin): Starts working in 2-4 hours, peaks in 4-12 hours, and lasts for 12-18 hours. Provides background insulin coverage.
- Long-acting insulin: Starts working after several hours and lasts for up to 24 hours or longer, providing basal (background) insulin coverage.
- Ultra-long-acting insulin: Provides basal insulin coverage for more than 24 hours, with a relatively flat action profile.
- Premixed insulin: Combinations of different types of insulin in a fixed ratio.
- Insulin Delivery Methods:
- Insulin Syringes and Vials: Traditional method using syringes to draw insulin from vials and inject it subcutaneously (under the skin).
- Insulin Pens: Pre-filled, pen-like devices that deliver measured doses of insulin through a fine needle. Pens are more convenient and discreet than syringes for many people.
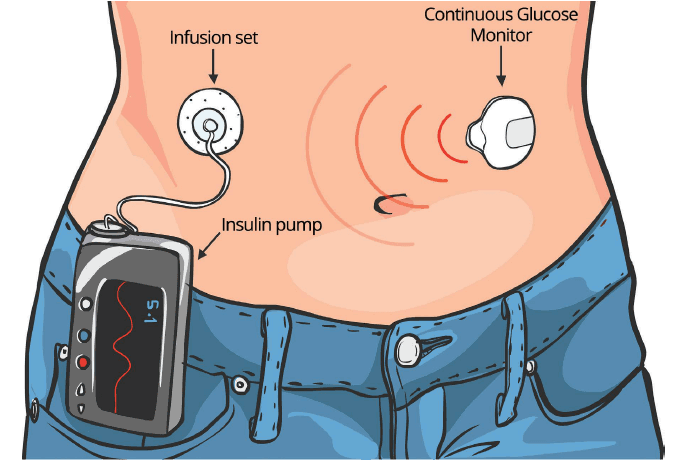
- Insulin Pumps: Small, computerized devices that continuously deliver basal insulin and bolus doses (mealtime or correction doses) through a catheter inserted under the skin. Insulin pumps offer more precise insulin delivery and flexibility. Figure 3 below illustrates an insulin pump.
Figure 3: Insulin Pump for Diabetes Management
Medication Adherence and Safety
Medication adherence is crucial for achieving the intended benefits of diabetes medications and insulin therapy. Following prescribed dosages, timing, and administration instructions is essential for healthy living with diabetes.
- Understand Your Medications: Know the names of your medications, their purpose, dosage, timing, and potential side effects. Ask your doctor or pharmacist any questions you have about your medications.
- Establish a Routine: Develop a consistent daily routine for taking your medications, especially for medications taken at specific times or with meals. Use reminders (alarms, pillboxes) if needed.
- Monitor for Side Effects: Be aware of potential side effects of your medications and report any concerns to your healthcare provider. Do not stop taking medication without consulting your doctor.
- Hypoglycemia Awareness and Management: If you take insulin or certain diabetes medications (e.g., sulfonylureas), be aware of the signs and symptoms of hypoglycemia and know how to treat it promptly. Carry a source of fast-acting carbohydrate.
Working with Your Healthcare Team
Effective diabetes management, especially when medication or insulin therapy is involved, requires close collaboration with your healthcare team.
- Regular Doctor Appointments: Attend scheduled doctor appointments for monitoring your diabetes, reviewing your medication regimen, and addressing any concerns.
- Certified Diabetes Educator (CDE): A CDE can provide comprehensive education on diabetes management, medication administration, blood sugar monitoring, lifestyle modifications, and problem-solving.
- Registered Dietitian (RD): An RD can help you develop a personalized meal plan that aligns with your medication regimen and overall health goals.
- Pharmacist: Your pharmacist can answer questions about your medications, potential drug interactions, and proper storage.
- Emergency Preparedness: Discuss an emergency plan with your healthcare team for situations like illness, surgery, or travel, which may require adjustments to your medication or insulin regimen.
Medication and insulin therapy are powerful tools in healthy living with diabetes. When used appropriately, in combination with healthy lifestyle choices and under the guidance of a healthcare team, they can significantly improve blood sugar control, reduce the risk of complications, and enhance quality of life.
7. Preventing and Managing Diabetes Complications Through Healthy Living
Common Diabetes Complications and Their Risks
Uncontrolled diabetes over time can lead to a range of serious complications affecting various parts of the body. However, proactive healthy living with diabetes can significantly reduce the risk and progression of these complications. Common diabetes complications include:
- Cardiovascular Disease: Heart disease and stroke are leading causes of death in people with diabetes. Diabetes increases the risk of atherosclerosis (plaque buildup in arteries), high blood pressure, and abnormal cholesterol levels.
- Neuropathy (Nerve Damage): High blood sugar can damage nerves throughout the body, leading to various types of neuropathy. Peripheral neuropathy affects the hands and feet, causing pain, numbness, tingling, and loss of sensation. Autonomic neuropathy affects involuntary functions like digestion, heart rate, and bladder control.
- Nephropathy (Kidney Disease): Diabetes is a leading cause of kidney failure. High blood sugar can damage the small blood vessels in the kidneys, impairing their filtering function.
- Retinopathy (Eye Damage): Diabetes can damage the blood vessels in the retina, the light-sensitive lining of the eye, leading to vision loss and blindness. Diabetic retinopathy is a leading cause of blindness in adults.
- Foot Problems: Neuropathy and poor circulation in the feet increase the risk of foot ulcers, infections, and amputations. Even minor foot injuries can become serious if not properly managed.
- Skin Conditions: People with diabetes are more prone to skin infections, bacterial and fungal infections, and dry, itchy skin.
- Hearing Impairment: Studies suggest that diabetes may increase the risk of hearing loss.
- Alzheimer’s Disease: Research suggests a link between diabetes and an increased risk of Alzheimer’s disease and cognitive decline.
Lifestyle Strategies to Minimize Complication Risks
Adopting healthy living with diabetes strategies is the most effective way to minimize the risk of developing or progressing diabetes complications.
- Maintain Optimal Blood Sugar Control: The cornerstone of complication prevention is keeping blood sugar levels as close to target ranges as safely possible. This involves consistent blood sugar monitoring, following your meal plan, exercising regularly, and taking medications as prescribed.
- Manage Blood Pressure: High blood pressure significantly increases the risk of cardiovascular disease and kidney disease in people with diabetes. Aim to keep blood pressure within target ranges (often below 130/80 mmHg) through lifestyle modifications and medication if needed.
- Manage Cholesterol Levels: High LDL (“bad”) cholesterol and triglycerides, and low HDL (“good”) cholesterol are common in diabetes and increase cardiovascular risk. Lifestyle modifications (healthy diet, exercise) and medications (statins) may be needed to manage cholesterol levels.
- Quit Smoking: Smoking significantly worsens diabetes complications, especially cardiovascular disease, neuropathy, and retinopathy. Quitting smoking is one of the most important steps for healthy living with diabetes.
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight, particularly for Type 2 diabetes, can improve insulin sensitivity, blood sugar control, and reduce the risk of complications.
- Healthy Diet: Follow a diabetes-friendly diet rich in fruits, vegetables, whole grains, and lean protein, low in saturated and trans fats, added sugars, and processed foods.
- Regular Exercise: Engage in regular physical activity to improve insulin sensitivity, blood sugar control, cardiovascular health, and weight management.
- Stress Management: Practice stress reduction techniques to minimize the impact of stress on blood sugar levels and overall health.
- Foot Care: Practice daily foot care, including washing and drying feet thoroughly, inspecting feet for cuts, blisters, or redness, moisturizing dry skin (but not between toes), and wearing comfortable, supportive shoes. Get regular foot exams by a podiatrist.
Regular Health Check-ups and Screenings
Regular health check-ups and screenings are crucial for early detection and management of diabetes complications. These should be part of your healthy living with diabetes routine.
- Annual Eye Exam (Dilated): Get a dilated eye exam annually by an ophthalmologist or optometrist to screen for diabetic retinopathy.
- Annual Kidney Function Tests: Get annual urine and blood tests to assess kidney function (urine albumin and eGFR).
- Annual Comprehensive Foot Exam: Have a comprehensive foot exam annually by a podiatrist, and more frequently if you have risk factors for foot problems.
- Regular Blood Pressure Checks: Get your blood pressure checked at each doctor visit, and monitor at home if recommended.
- Lipid Panel (Cholesterol and Triglycerides): Get your lipid panel checked at least annually, or more frequently if you have abnormal results.
- A1c Test (HbA1c): Get your A1c test done at least twice a year, or more frequently as recommended by your doctor, to assess long-term blood sugar control.
- Dental Check-ups: Get regular dental check-ups and cleanings to prevent and manage gum disease, which is more common and severe in people with diabetes.
Early Detection and Intervention
Early detection and intervention are key to minimizing the impact of diabetes complications. By being proactive about healthy living with diabetes and attending regular check-ups, you can identify potential problems early and take timely action to prevent or slow down their progression.
- Report Any New Symptoms: Be vigilant about reporting any new symptoms or changes in your health to your doctor promptly. Don’t ignore seemingly minor symptoms, as they could be early signs of a complication.
- Adhere to Treatment Recommendations: Follow your healthcare team’s recommendations for medication, lifestyle modifications, and follow-up appointments. Adherence is crucial for effective management.
- Education and Self-Management: Continue to educate yourself about diabetes and its complications. The more you know, the better equipped you are to manage your condition and advocate for your health.
By embracing healthy living with diabetes and being proactive about prevention, early detection, and management, you can significantly reduce your risk of complications and live a long and healthy life.
Frequently Asked Questions about Healthy Living with Diabetes
What is the best diet for someone with diabetes?
How much exercise do I need if I have diabetes?
How often should I check my blood sugar?
What are the signs of low blood sugar (hypoglycemia)?
Can diabetes be reversed with healthy living?
Is it safe for people with diabetes to eat fruit?
How can I manage stress with diabetes?
What are the long-term complications of diabetes?
What is A1c and what is the target range for diabetes?
Where can I find more support and resources for healthy living with diabetes?
9. Conclusion: Embracing a Healthy and Fulfilling Life with Diabetes
Living with diabetes is undoubtedly a journey that requires commitment, knowledge, and proactive self-care. However, it is absolutely possible to thrive and live a healthy and fulfilling life with diabetes. Healthy living with diabetes is not about limitations; it’s about empowerment. It’s about making informed choices that support your well-being and enable you to take control of your health.
This comprehensive guide has explored the essential pillars of healthy living with diabetes, from the foundational role of nutrition and physical activity to the critical importance of blood sugar monitoring, stress management, and proactive complication prevention. By embracing these strategies, you are not merely managing a condition; you are actively building a healthier future for yourself. Remember that small, consistent steps, informed by knowledge and supported by your healthcare team and loved ones, will lead to significant positive changes over time.
Healthy living with diabetes is a personalized journey. Find what works best for you, be kind to yourself, and celebrate your progress along the way. Embrace the power of knowledge, the strength of self-care, and the support of your community. By doing so, you can confidently navigate life with diabetes and achieve your fullest potential for health and happiness.
Share this article with someone who could benefit from learning more about healthy living with diabetes! Leave a comment below with your own tips or questions about managing diabetes – we’d love to hear from you and build a supportive community.
Diavetes.com



